What is Lyme Disease?
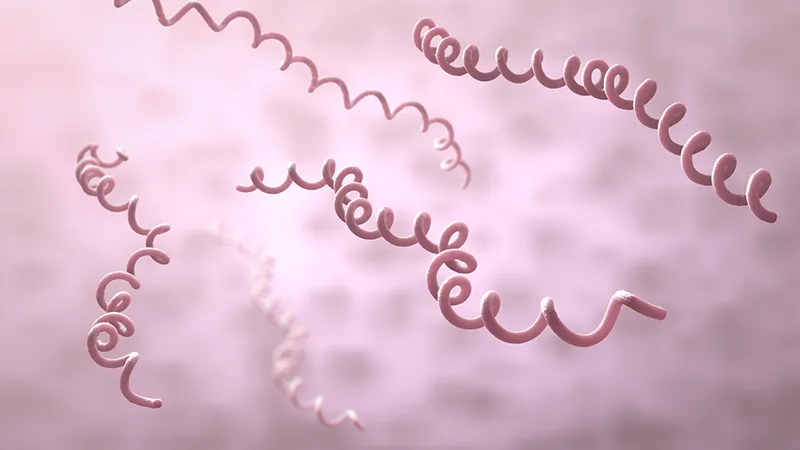
Lyme disease is a spirochetal bacterial infection which is transmitted predominantly by the bite of the Ixodes Scapularis tick, commonly referred to as the black-legged tick or deer tick.
The clinical symptoms of Lyme disease can vary from person to person at initial presentation and during the course of the infection. Symptoms ranging from a relatively benign skin rash to severe arthritic and neurological disabilities. Lyme disease occurs in stages with different clinical manifestations at each stage. Any organ system can be involved, but the bacteria commonly attack skin, joint, heart, and nerve tissue— including the brain.